Contraindication
- NEUPOGEN® is contraindicated in patients with a history of serious allergic reactions to human granulocyte colony-stimulating factors (G-CSFs), such as filgrastim or pegfilgrastim
Splenic Rupture
- Splenic rupture, including fatal cases, can occur following the administration of NEUPOGEN®
- Evaluate patients who report left upper abdominal or shoulder pain for an enlarged spleen or splenic rupture
Acute Respiratory Distress Syndrome (ARDS)
- ARDS has been reported in patients receiving NEUPOGEN®
- Evaluate patients who develop fever and lung infiltrates or respiratory distress for ARDS
- Discontinue NEUPOGEN® in patients with ARDS
Serious Allergic Reactions
- Serious allergic reactions, including anaphylaxis, have been reported in patients receiving NEUPOGEN®
- Majority of reported events occurred upon initial exposure
- Provide symptomatic treatment for allergic reactions
- Allergic reactions, including anaphylaxis, in patients receiving NEUPOGEN® can recur within days after the discontinuation of initial anti-allergic treatment
- Permanently discontinue NEUPOGEN® in patients with serious allergic reactions
Sickle Cell Disorders
- Severe and sometimes fatal sickle cell crises can occur in patients with sickle cell disorders receiving filgrastim products
- Discontinue NEUPOGEN® if sickle cell crisis occurs
Glomerulonephritis
- Has occurred in patients receiving NEUPOGEN®
- Diagnoses were based on azotemia, hematuria, proteinuria, and renal biopsy
- Generally, events resolved after dose reduction or discontinuation of NEUPOGEN®
- If causality is likely, consider dose-reduction or interruption of NEUPOGEN®
Alveolar Hemorrhage and Hemoptysis
- Alveolar hemorrhage, manifesting as pulmonary infiltrates and hemoptysis requiring hospitalization, have been reported in NEUPOGEN®-treated healthy donors undergoing peripheral blood progenitor cell (PBPC) collection mobilization
- Hemoptysis resolved with discontinuation of NEUPOGEN®
- The use of NEUPOGEN® for PBPC mobilization in healthy donors is not an approved indication
Capillary Leak Syndrome (CLS)
- CLS has been reported after G-CSF administration, including NEUPOGEN®
- Characterized by hypotension, hypoalbuminemia, edema, and hemoconcentration
- Episodes vary in frequency, severity, and may be life-threatening if treatment is delayed
- Patients with symptoms should be closely monitored and receive standard symptomatic treatment, which may include the need for intensive care
Myelodysplastic Syndrome and Acute Myeloid Leukemia (AML)
Patients with Severe Chronic Neutropenia
- Confirm the diagnosis of SCN before initiating NEUPOGEN® therapy
- MDS and AML have been reported to occur in the natural history of congenital neutropenia without cytokine therapy
- Cytogenetic abnormalities, transformation to MDS, and AML have also been observed in patients treated with NEUPOGEN® for SCN
- Based on available data including a postmarketing surveillance study, the risk of developing MDS and AML appears to be confined to the subset of patients with congenital neutropenia.
- Abnormal cytogenetics and MDS have been associated with the eventual development of myeloid leukemia
- The effect of NEUPOGEN® on the development of abnormal cytogenetics and the effect of continued NEUPOGEN® administration in patients with abnormal cytogenetics or MDS are unknown. Monitor patients for signs and symptoms of MDS/AML in these settings.
- If a patient with SCN develops abnormal cytogenetics or myelodysplasia‚ the risks and benefits of continuing NEUPOGEN® should be carefully considered
Patients with Breast and Lung Cancer
- MDS and AML have been associated with the use of NEUPOGEN® in conjunction with chemotherapy and/or radiotherapy in patients with breast and lung cancer. Monitor patients for signs and symptoms of MDS/AML in these settings.
Thrombocytopenia
- Thrombocytopenia has been reported in patients receiving NEUPOGEN®
- Monitor platelet counts
Leukocytosis
Patients with Cancer Receiving Myelosuppressive Chemotherapy:
- White blood cell counts ≥ 100,000/mm3 were observed in about 2% of patients who received NEUPOGEN® at dosages > 5 mcg/kg/day
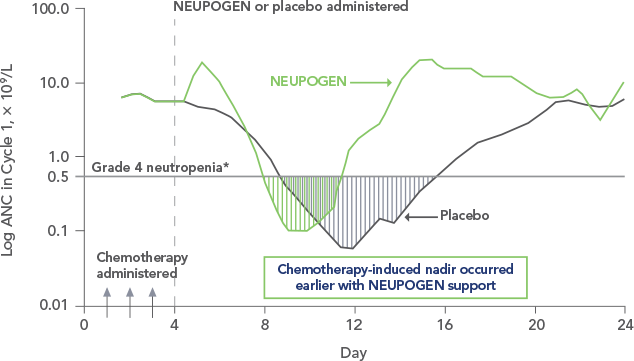
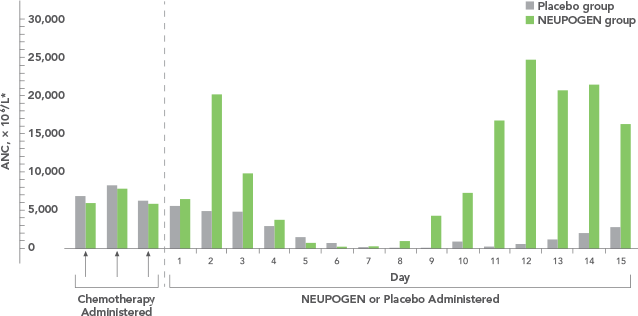
- Discontinue NEUPOGEN® if the absolute neutrophil count (ANC) surpasses 10,000/mm3 after the chemotherapy-induced ANC nadir has occurred
- Monitor CBCs at least twice weekly
- Dosages of NEUPOGEN® that increase the ANC beyond 10,000mm3 may not result in any additional clinical benefit
- Discontinuation of NEUPOGEN® therapy usually resulted in a 50% decrease in circulating neutrophils within 1 to 2 days, with a return to pretreatment levels in 1 to 7 days
Peripheral Blood Progenitor Cell Collection and Therapy (PBPC):
- Discontinue NEUPOGEN® if the leukocyte count rises to > 100,000/mm3
Cutaneous Vasculitis
- Moderate or severe cases of cutaneous vasculitis have been reported in patients treated with NEUPOGEN®
- Most reports involved patients with severe chronic neutropenia receiving long-term NEUPOGEN® therapy
- Hold NEUPOGEN® therapy in patients with cutaneous vasculitis
- NEUPOGEN® dose may be reduced when the symptoms resolve and the ANC has decreased
Potential Effect on Malignant Cells
- G-CSF receptor has also been found on tumor cell lines
- The possibility that NEUPOGEN® acts as a growth factor for any tumor type, including myeloid malignancies and myelodysplasia, cannot be excluded
- The safety of filgrastim in chronic myeloid leukemia (CML) and myelodysplasia has not been established
- When NEUPOGEN® is used to mobilize PBPC, tumor cells may be released from the marrow and subsequently collected in the leukapheresis product
- The effect on reinfusion of tumor cells has not been well studied, and the limited data available are inconclusive
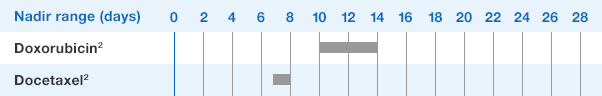
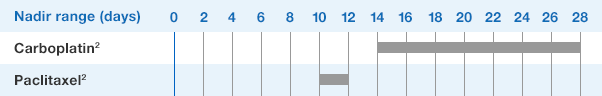
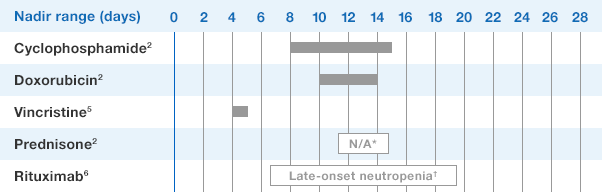
Simultaneous Use with Chemotherapy and Radiation Not Recommended
- The safety and efficacy of NEUPOGEN® given simultaneously with cytotoxic chemotherapy have not been established
- Do not use NEUPOGEN® 24 hours before or after administration of cytotoxic chemotherapy
- The safety and efficacy of NEUPOGEN® have not been evaluated in patients receiving concurrent radiation therapy
- Avoid the simultaneous use of NEUPOGEN® with chemotherapy and radiation therapy
Nuclear Imaging
- Increased hematopoietic activity of the bone marrow has been associated with transient positive bone-imaging changes
- Consider when interpreting bone-imaging results
Aortitis
- Aortitis has been reported in patients receiving NEUPOGEN®
- It may occur as early as the first week after start of therapy
- Manifestations may include generalized signs and symptoms such as fever, abdominal pain, malaise, back pain, and increased inflammatory markers (e.g., c-reactive protein and white blood cell count)
- Consider aortitis in patients who develop these signs and symptoms without known etiology. Discontinue NEUPOGEN® if aortitis is suspected.
The most common adverse reactions in patients:
- with nonmyeloid malignancies receiving myelosuppressive anti-cancer drugs are anemia, constipation, diarrhea, oral pain, vomiting, asthenia, malaise, edema peripheral, hemoglobin decreased, decreased appetite, oropharyngeal pain, and alopecia
- with AML are epistaxis, back pain, pain in extremity, erythema, rash maculo-papular, diarrhea, constipation, and transfusion reaction
- with nonmyeloid malignancies undergoing myeloablative chemotherapy followed by BMT are rash, hypersensitivity, thrombocytopenia, anemia, hypertension, sepsis, bronchitis, and insomnia
- undergoing peripheral blood progenitor cell mobilization and collection are bone pain, pyrexia, increased blood alkaline phosphatase, and headache
- with severe chronic neutropenia are arthralgia, bone pain, back pain, muscle spasms, musculoskeletal pain, pain in extremity, splenomegaly, anemia, upper respiratory tract infection, urinary tract infection, epistaxis, chest pain, diarrhea, hypoesthesia, and alopecia
Please see NEUPOGEN® full Prescribing Information.
Indications
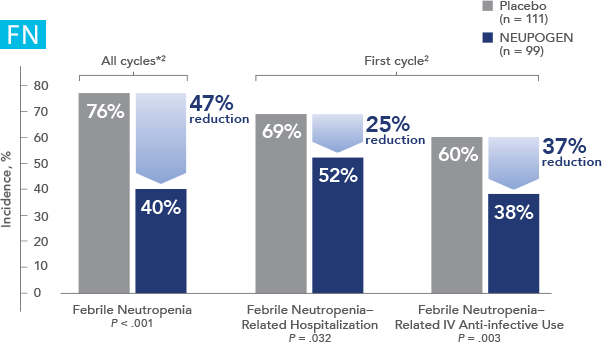
Patients with Cancer Receiving Myelosuppressive Chemotherapy
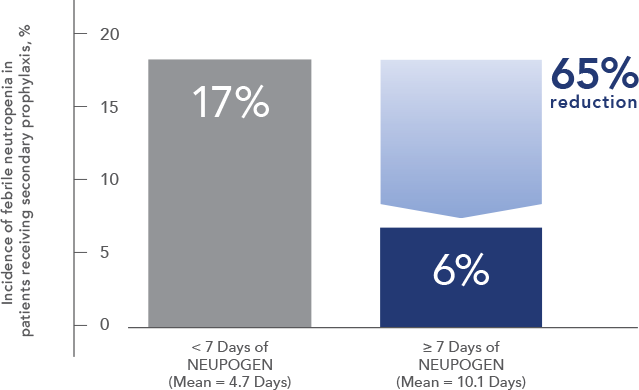
NEUPOGEN® is indicated to decrease the incidence of infection‚ as manifested by febrile neutropenia‚ in patients with nonmyeloid malignancies receiving myelosuppressive anti-cancer drugs associated with a significant incidence of severe neutropenia with fever.
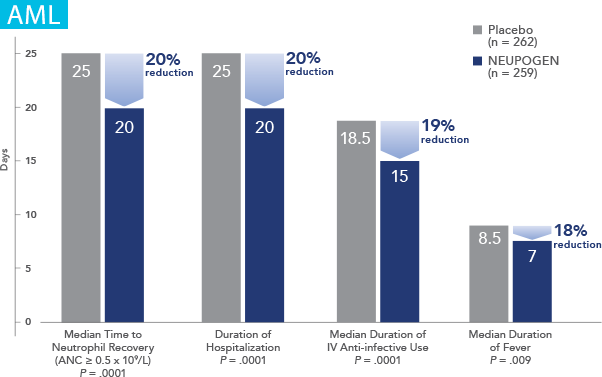
Patients with Acute Myeloid Leukemia Receiving Induction or Consolidation Chemotherapy
NEUPOGEN® is indicated for reducing the time to neutrophil recovery and the duration of fever, following induction or consolidation chemotherapy treatment of patients with acute myeloid leukemia (AML).
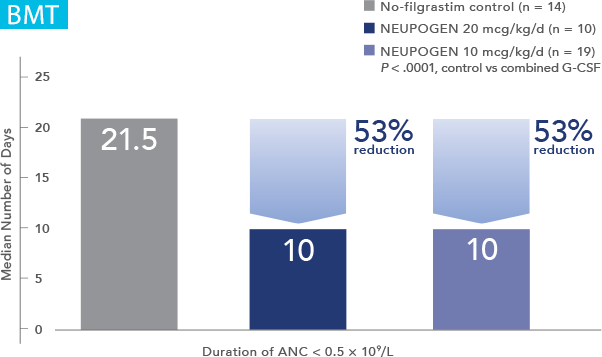
Patients with Cancer Undergoing Bone Marrow Transplantation
NEUPOGEN® is indicated to reduce the duration of neutropenia and neutropenia-related clinical sequelae‚ e.g. febrile neutropenia, in patients with nonmyeloid malignancies undergoing myeloablative chemotherapy followed by bone marrow transplantation.
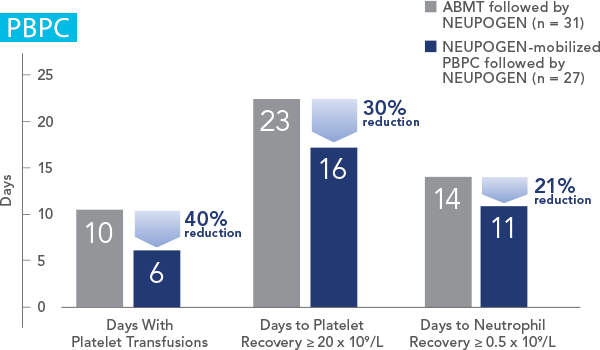
Patients Undergoing Autologous Peripheral Blood Progenitor Cell Collection and Therapy
NEUPOGEN® is indicated for the mobilization of autologous hematopoietic progenitor cells into the peripheral blood for collection by leukapheresis.
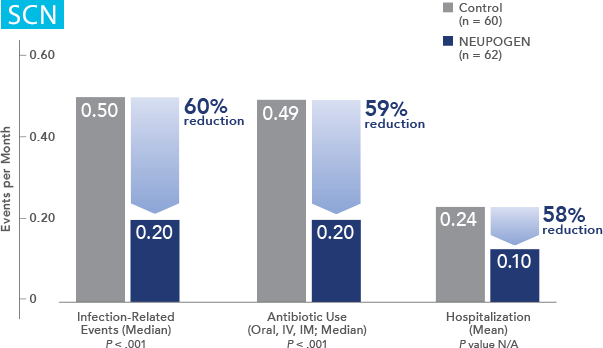
Patients with Severe Chronic Neutropenia
NEUPOGEN® is indicated for chronic administration to reduce the incidence and duration of sequelae of severe neutropenia (e.g.‚ fever‚ infections‚ oropharyngeal ulcers) in symptomatic patients with congenital neutropenia‚ cyclic neutropenia‚ or idiopathic neutropenia.